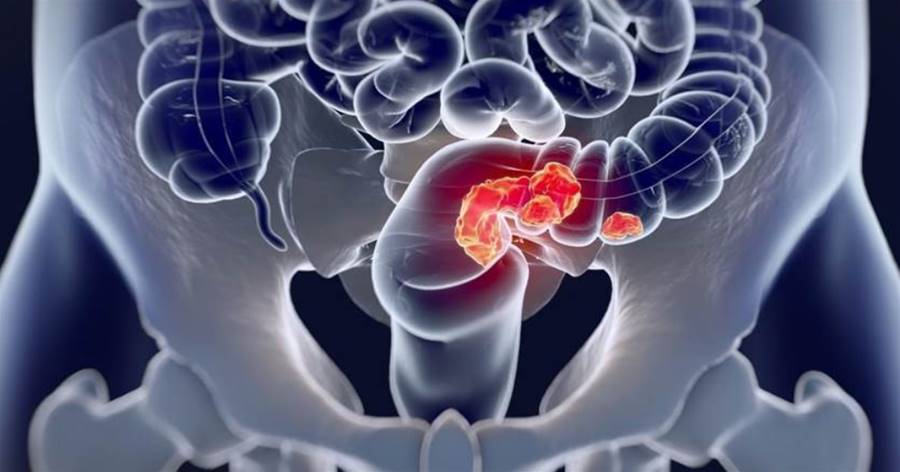
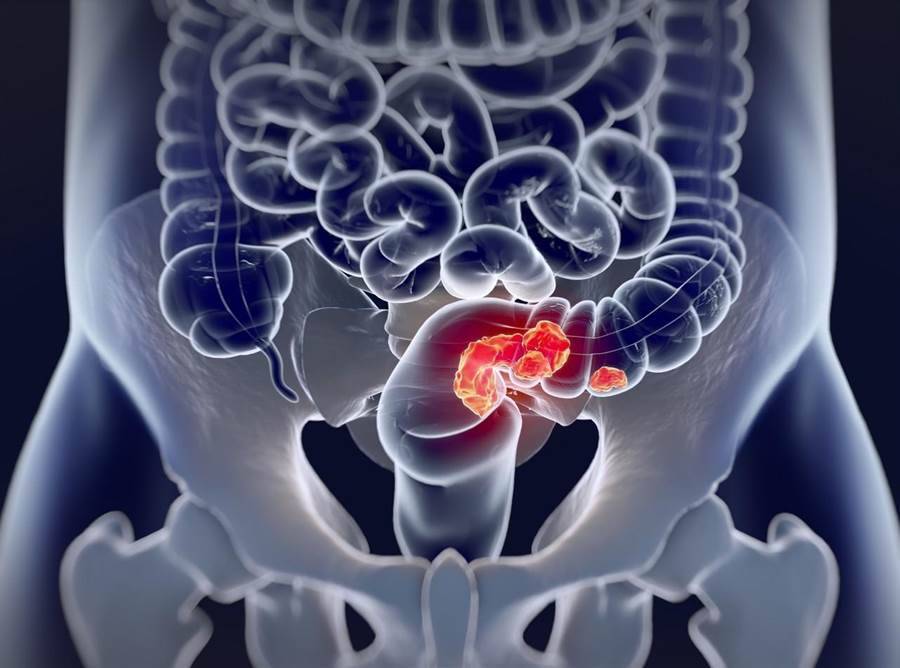
Colorectal cancer is a disease with an increasing incidence. Environmental factors and genetic factors are known to increase the likelihood of colorectal cancer. Most colorectal cancer patients are members of families with hereditary colon cancer syndrome. , inflammatory bowel disease with a personal or family history of colorectal cancer or adenomas, and greater abdominal radiation exposure.

What are the risk factors for colorectal cancer?1. Genetic factorsSeveral specific genetic diseases with extremely high risk of colon cancer have been identified. Most of these diseases are autosomal dominant, but only account for about 5% of colorectal cancer cases. Familial adenomatous polyposis is the most common familial colon cancer syndrome, and polyposis and its variants account for less than 1% of colorectal cancers.
In classic polyposis, many colon adenomas develop during childhood.
The average age at onset of symptoms is approximately 16 years, and 90% of untreated individuals develop colon cancer before the age of 45. Although attenuating polyposis is associated with a higher risk of colon cancer, it is characterized by fewer adenomas and an older average age at diagnosis.
2.
The article is not finished. Click on the next page to continue.
The article is not finished. Click on the next page to continue.
Next page


















