
Is colon cancer hereditary?Doctors say there is a genetic susceptibility to cancer. Research has also found that cancer has regional or family aggregation. Patients with hereditary cancers carry genetic material that makes their cells more likely to become cancerous and may be passed on to the next generation.
At present, about 20% of cancers are hereditary in families. However, not all cancers are hereditary, and only 5% to 10% of tumors are hereditary.
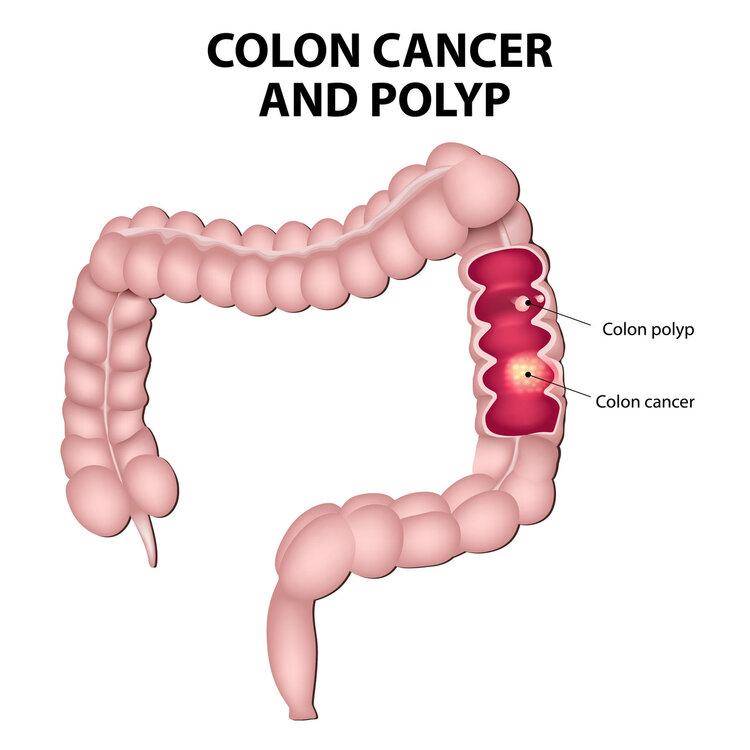
Among them, colon cancer has a hereditary risk.

There are two inheritance pathways for colon cancer. One is hereditary precancerous colon polyps, accounting for about 1% to 2%; the other is hereditary non-polyposis colon cancer, and the inactivation of nucleic acid repair genes in human genetic material. Related, to put it simply, cancer genes are directly passed on to the next generation, accounting for about 2% to 7%.
A large number of studies have shown that if there is a colon cancer patient in a family, the probability of blood relatives, such as parents, children, brothers and sisters, etc., to develop colon cancer is significantly increased, which is about 2 to 3 times that of ordinary people.
In addition to genetics, these factors may also easily induce colon cancerColon cancer occurs under the influence of a variety of carcinogenic factors.
The article is not finished. Click on the next page to continue.
The article is not finished. Click on the next page to continue.
Next page


















